COVID-19 Weekly Briefing for Monday, March 21, 2022
Fasting makes you healthy; a one-month COVID-19 forecast: BA.2 is on the way.
People without insurance will no longer be covered for COVID-19 (C19) testing, treatment, or vaccination; new information informs our understanding of weight loss; brace for it: a new wave of C19 is likely on the way; longer inter-dose intervals improved the effectiveness of C19 vaccination (not news to us); more hospital staffing shortages; and the CDC changes it’s algorithm for assessing community risk (again) to skew it even further to focusing exclusively on hospitalizations and deaths (rather than cases).
This week’s Briefing begins with an announcement for the office:
On March 22, 2022, at 11:59 pm ET, the HRSA COVID-19 Uninsured Program will stop accepting claims for testing and treatment due to a lack of sufficient funds.
On April 5, 2022, at 11:59 pm ET, the HRSA COVID-19 Uninsured Program will also stop accepting vaccination claims due to a lack of sufficient funds.
I. Weight loss and total energy expenditure (TEE): the intriguing new science of energy envelopes and fasting
An age-dependent energy envelope
1558 - 1568. It is widely believed that excess fat on our bodies reflects an imbalance between the amount of energy (measured in calories or kcal) that we consume vs. the amount we burn. And that diet is the chief driver of energy consumption while activity and lifestyle are the chief drivers of energy expenditure.
According to this line of thinking, if a sedentary person eats the same number of calories as an exerciser, we would expect that the sedentary person would burn fewer calories and store more fat compared to the exerciser.
But new research is showing that, while diet does determine energy intake, activity might not be a critical driver of total energy expenditure (TEE). For one thing, regardless of lifestyle or activity, it has now been established that how many calories we burn each day is highly age-dependent.
TEE ramps up during infancy when our brains and immune systems are developing, then starts to drop until we reach our mid-20s. At that point, it stabilizes throughout early and middle adulthood, dropping again with each decade of life beginning at about age 60.
This lowering of metabolism helps explain the difficulty many of us have trying to lose weight as we age. And this is true regardless of whether we are physical laborers or accountants; receptionists in San Diego or hunter-gatherers in rural Africa; exercise addicts or couch potatoes.
It turns out most of our TEE is linked to automatic ongoing ‘basal activities’ like digesting food, pumping blood, and mediating inflammatory processes in areas of the body under stress, and to relatively low-exertion activities such as thinking (in humans, brain activity accounts for about 20% of TEE), moving from one room to another, and fidgeting, rather than to occasional exertions like taking a run or mowing the lawn.
We now understand that the body regulates energy expenditure according to an internally calculated daily allotment–an ‘energy envelope’–based on age, and it is hard to burn more or fewer calories than the age-dependent, pre-allotted amount.
If, for example, we use a lot of energy during a workout, our bodies try to make up for that by spending fewer calories on other things (like generating an inflammatory response) in order to stay within the daily TEE allotment.
Our bodies also adapt physiologically to regular exercise, becoming more efficient over time, burning fewer and fewer calories during exertion. For example, in one study, sedentary women who trained to run a half marathon increased their TEE at first but after a few weeks, gradually dropped back to about the same TEE as before they had started to train. This is hormesis at work. The body is getting stronger and more efficient by repeatedly stressing it in a consistent way over time.
Of course, it is possible to push through the limitations of our energy envelope with more extreme degrees of exertion. People who routinely exercise for many hours per day such as ultramarathon runners, Olympic swimmers, and Ironman triathletes can push TEE beyond the envelope to induce weight loss. But even during extreme endurance activities, we quickly reach an upper limit to how many calories we can burn–about 2.5 times the basal metabolic rate (BMR) which is the amount we burn at rest.
This has repercussions for health–especially with regard to weight loss. After 34 years in clinical practice, it is abundantly clear to me that while exercise is a critical hormetic practice that strengthens the heart, lungs, and muscles, promoting longer lifespan and healthspan, it is not a good strategy for weight loss. If we can’t (without dedicating many hours each day) exercise our way to an ideal body weight, then weight loss must be driven chiefly by our diet.
Why diets fail
The strategy of most weight loss programs like Weight Watchers, Jenny Craig, and even Optavia (the program we use at the office) is to tilt the balance between calories consumed and calories burned. Taking in fewer calories while keeping activity levels constant can, in the short term, induce weight loss.
But calorie restriction diets only work for a while. After about 3-4 months, the weight loss hits a plateau. At this point, even if someone is consuming less than half their normal amount of calories, they will struggle to lose any more weight.
That’s because, over time, our bodies adapt to lower food intake by adjusting down our metabolism. A 30-year-old who spends too much time on a calorie restriction diet can lower her metabolic rate to a level comparable to a 70-year-old, and that’s bad. To make matters worse, when this happens it becomes very difficult to raise metabolism again–sadly, it doesn’t automatically adjust back upward when we resume eating more calories.
When weight loss stops (due to slowed metabolism), we lose the feeling of reward that came with the initial good results. This leads most people to (understandably) drop the diet. And when they return to the eating habits developed over a lifetime–only now, in the context of a slower metabolism–they gain weight quickly.
Research shows that roughly 80% of people who lose significant weight on calorie-restriction diets, with or without exercise, will begin to regain their weight within the first year of coming off their diet and will regain, on average, more than half of what they lost within two years.
A better strategy
At our clinic, we use Optavia (the all-natural version of Medifast) short-term to initiate rapid weight loss but then transition patients to a high-fiber, low-glycemic-load diet (HFLG) that resembles what is commonly referred to as the Mediterranean diet.
When patients transition from the standard American diet (or from a calorie restriction diet) to an HFLG, they report better mental acuity, sleep quality, and overall feeling of wellbeing. Why? An HFLG diet keeps blood sugar stable. Most calorie restriction diets drive blood sugar too low and that doesn’t feel good (more about this below).
HFLG also improves the gut microbiome–the trillions of microorganisms that live inside our digestive systems and inform our health in ways ranging from immunity to mood. I will expound on the gut microbiome in a future Weekly Briefing but for now, suffice it to say that diets without very high amounts of naturally occurring plant fiber are a key driver of obesity, diabetes, cardiovascular disease, and other forms of chronic illness because they deprive the gut microbiome of their food source: fiber. Without fiber, the healthy bacteria in our gut die-off leaving our health weakened.
Establishing comfort on an HFLG diet is both the prelude to the next phase of weight loss and half of the blueprint for the style of eating that patients are encouraged to maintain long-term after they’ve reached the weight at which they feel healthy and comfortable. But before they get to that point, there is still one more piece to the puzzle of successful long-term healthy weight management to be put in place: fasting.
Fasting
In recent years, intermittent fasting or time-restricted eating (also known as ‘the 16/8 method’) has become a popular weight loss technique. There are many versions of fasting being promoted in books and on the internet. Some make sense scientifically, many do not.
For the purpose of this discussion, intermittent fasting refers to taking in no calories for 24 or more continuous hours. This is something I have employed both personally and in my practice for many years. But there is a lot of misinformation regarding how it works and how to fast correctly.
It may seem strange but our bodies respond very differently to calorie restriction than to fasting. Unless we are on a highly carbohydrate-restricted diet, blood sugar can dip low enough during calorie-restricted diets to cause fatigue, headache, light-headedness, extreme hunger, and impaired concentration.
Counter-intuitively, fasting (taking in no calories at all) does not drive blood sugar down too low. Fasting also does not induce extreme hunger. It preserves our energy and in most people, improves mental clarity. In addition, as mentioned above, prolonged calorie restriction induces a slowing of metabolism which leads to weight gain after coming off the diet. But fasting does not slow down metabolism. Why?
When you eat, your pancreas releases insulin to put the body into a state of energy storage. Insulin signals cells in the muscles and liver to take in glucose (sugar) absorbed from food and convert it into glycogen, the stored form of glucose that acts as a ready energy reserve. It also signals fat cells to convert glucose into triglycerides and store those as adipose or body fat. And it directs liver, muscle, and fat cells to shut down the release of stored energy for use by the body. In short, when you eat your body makes insulin and insulin is a hormone that promotes calorie storage while blocking calorie-burning.
Let’s imagine that your body’s TEE envelope is 2,000 kcal/day when you begin a calorie restriction diet. Prior to dieting, you had been consuming 2,500 kcal/day, on average, and had been gaining about 5 lbs. each year. If the (non-ketogenic) diet involves eating several times each day, that keeps insulin levels relatively high since you release insulin each time that you eat, and the effect of insulin on cells continues for 1-2 hours after a meal. So, even though you are restricting your intake to just 1,000 kcal/day, you don’t have access to the stored calories in glycogen (liver and muscles) or triglycerides (fat) because the regular secretion of insulin won’t allow it! The result is a 1,000 kcal deficit that results in extreme hunger, fatigue, and other unpleasant symptoms until, eventually, metabolism slows down to meet the chronically reduced caloric availability of the diet.
Summing up: regular eating while restricting calories means high insulin levels which block access to stored energy and drives blood sugar way down. That doesn’t feel good. And having access to just the 1,000 kcal that you are eating causes metabolism to adjust downward, setting you up for weight gain once you come off the diet and go back to consuming a more normal amount of calories.
By contrast, fasting does not cause the body to produce insulin. In fact, during fasting, insulin levels drop. That signals cells in the liver and muscles to start breaking down glycogen into glucose and releasing it into the blood for energy. It also signals fat cells to do the same with regard to their stored triglycerides, breaking them down into glycerol and free fatty acids which are converted in the liver to ketone bodies which are an alternative energy source to sugar.
Lowering insulin through fasting enables us to maintain our normal TEE, keeping metabolism from slowing while burning fat, losing weight, and feeling well on a steady supply of energy.
Summing up: when you fast, you lower insulin and your body starts to eat its own stored energy, keeping metabolism from dropping and inducing weight loss.
More benefits to fasting: hormesis
In a recent briefing, I discussed the concept of hormesis, the physiological process whereby we grow stronger in response to repeated exposure to a particular stressor. I discussed how regular exercise and other practices such as sauna bathing have been shown to improve both lifespan and healthspan. Fasting is another hormetic practice. How does it work?
The cells of our body contain several distinct membrane-bound structures called organelles, each of which acts like a miniature organ doing its own special work that the cell relies upon to function properly. For example, the mitochondrion is an organelle that has the function of producing energy; the lysosome has the function of breaking large molecules down into smaller ones; and phagosomes are organelles that capture and eliminate foreign or toxic material such as viral proteins.
As we age, organelles like mitochondria and lysosomes start to lose energy and become less efficient. We also make fewer phagosomes as we age which lowers our self-protection. These organelles can collect toxins and proteins that are defective (unfoldable) and unusable, mucking up their ability to perform their specialized jobs. Cells containing significantly dysfunctional organelles are referred to as senescent cells.
After about 24 hours without taking in any calories (there is variation between people and it may also depend on when during the day you fast), we enter the hormetic fasting state which induces the production of a special kind of phagosome called an autophagosome.
Autophagosomes help repair or digest dysfunctional organelles within senescent cells as a way of extracting needed energy from them during fasting. They swallow up waste, attach themselves to lysosomes whose job is to break big molecules down into smaller ones, and then feed the cell by degrading these senescent organelles to release energy–a process known as autophagy.
Autophagy can be thought of as the body’s way of keeping energy levels high during cellular starvation and also as a way of getting healthier and stronger by clearing out toxic and dead materials to improve the quality and function of organelles within our cells. This is why people who fast regularly often look much younger than their age.
Fasting dramatically increases the number of autophagosomes within cells, driving autophagy. The longer we fast, the more autophagosomes we make, and the healthier and ‘younger’ our cells become. Of course, there are limits to fasting as there are to all hormetic practices. I personally fast for 24-26 hours 2-3 times per week and for 48-72 hours about once every 2-3 months. Many studies have demonstrated that fasting extends lifespan.
Studies vary in terms of how long a fast is required to increase the production of autophagosomes to induce autophagy. Some studies indicate autophagy may begin as soon as 16-20 hours without any calories. Most studies suggest it takes closer to 24 hours of fasting to induce autophagy. And it looks like the rate of autophagy continues to increase during prolonged periods of fasting, reaching peak levels at about 2 - 3 days. It also seems that fasting during the night may promote more autophagy than daytime fasting so, for example, fasting from breakfast to breakfast may induce more autophagy than from lunch to lunch or dinner to dinner.
Fasting is part of our evolution
Humans evolved over a period of about 6 million years, during which time we lived by a rhythm of feasting and fasting that was necessitated by our natural environment. During cold seasons, floods, droughts, or other environmentally hostile periods when little plant food was available for consumption, humans would often go days or longer before they were able to kill an animal and feast for a day or two, surviving in the interim on just water and whatever calories they had been able to store in their bodies.
Because of this feasting-and-fasting pattern of eating, our bodies evolved to become excellent at storing fat. That served us well throughout most of our evolutionary history when calories were often scarce. But now, amidst unprecedented abundance, both in terms of the density of calories in today’s extremely carbohydrate-rich processed foods and the everpresent availability of things to eat in advanced societies like ours, this evolutionary advantage is working against us.
For nearly all of our history as a species, getting enough to eat was our greatest day-to-day challenge. Now, one of our greatest challenges is learning how not to eat too much.
Autophagy is an evolutionary adaptation. A way of promoting health and self-preservation by utilizing the reserve energy of intracellular toxins and debris to feed starving cells while cleaning them out and bringing them back to optimal smooth functioning.
When modern societies conceived of the ‘three square meals a day’ pattern of eating, this represented an attempt to ensure that all citizens were afforded adequate nutrition. We didn’t know it then, but this rhythm of feeding, designed to put an end to malnutrition, closed us off from the hormetic practice of fasting which had been part of human societies for millions of years.
And today, with food not only exceedingly available but also manufactured to be hyper-delicious (to the point of driving ‘soft addictions’), most people eat more than three times per day, supplementing their meals with snacks–some of which are taken strictly for pleasure. And many of us now habitually each throughout the day to soothe anxiety, loneliness, boredom, or stress. Snack food manufacturers have succeeded in promoting this as part of a lifestyle and have even invented the concept of ‘healthy snacking’ as if supplementing meals with better quality food could make snacking a health practice. But we now know that the opposite is true. Snacking drives up insulin and insulin blocks fat burning. Snacking is making us fat.
Fasting is more than a tool for weight loss, it’s a health practice
When we lose weight through fasting, we maintain our metabolic rate, burn fat, enjoy good energy and mental clarity. Fasting turns on autophagy, reversing our biological age, and induces the production of hormones called sirtuins that have been shown to protect against cancers and extend lifespan. Weight loss achieved through fasting is less likely to result in rebound weight gain, feelings of misery during the weight loss period, or the development of stretch marks once the fat goes away.
Fasting, it can be said, is a tool for health and happiness. It stresses the body hormetically, making it stronger and healthier when done consistently over time. It has been a traditional practice among many cultures and a spiritual practice among many different religions. It promotes a kind of physiological cleansing at the cellular level, the benefits of which can be felt almost immediately among those who commit to doing it.
Of course, there are many more details, the articulation of which are not well-suited to the format of a Weekly Briefing. For those interested in learning more, feel free to reach out. For now, let’s summarize by saying that combining fasting with a Mediterranean-style HFLG diet is the ultimate goal of our weight loss program which is designed to promote health, increase lifespan, and, perhaps most importantly of all, be sustainable over time.
II. BA.1 (Omicron), BA.2, BA2.2, BA.2.3, and future variants: where are things headed in the next few weeks?
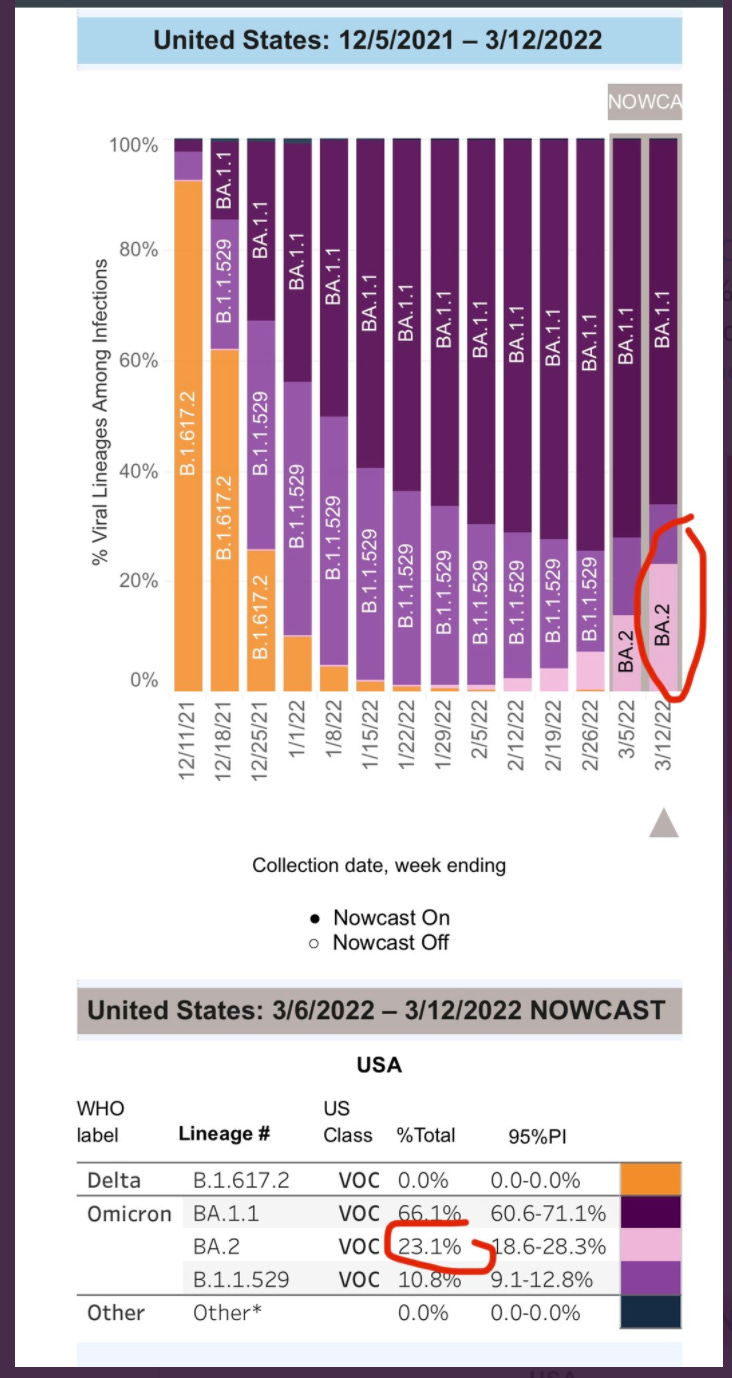
1569 - 1584. We are seeing new waves in cases driven by BA.1 (Omicron) and BA.2 in several countries in Asia and Europe. BA.2 is outcompeting BA.1 and is likely to replace it soon, globally. In the meantime, still more sublineages of Omicron have been identified around the world, including BA.2.2 and BA.2.3. What does all this mean for us in the coming weeks?
Let’s look at South Korea (SK) and Hong Kong (HK), both of which are currently in the midst of their biggest waves of the pandemic so far, with SK lagging a couple of weeks behind HK.
Both have astonishingly high case rates but the death rates are not at all comparable:
What’s happening here? Why is Hong Kong having such a high case mortality rate when it’s wave was similar (even a little smaller) compared to SK?
There are some important differences between HK and SK which likely inform the disconnect:
The booster rate (3 shots) is 63% in SK compared to HK where it is just 30%
The primary vaccination rate (2 shots) is 87% in SK compared to HK where it is just 60% with more than half of people in HK over age 70 unvaccinated.
BA.2 is driving about 26% of cases in SK but accounts for nearly all new cases in HK (lavender) where the newest sub-variant BA.2.2 is also in the mix:
So far, we don’t have conclusive data to show whether or not BA.2 or BA.2.2 (or BA.2.3) are more virulent than BA.1 (Omicron). We know that BA.2 spreads faster than Omicron (about 30-40%) but at least so far, most authorities don’t believe it to be more deadly.
That said, there are early reports out of Asia including one compelling animal study from Japan indicating that BA.2 may attack the lungs more than BA.1 does. That’s not good. One important reason why Omicron is less virulent than prior variants is that it preferentially attacks the upper airways (nose and throat) rather than the lower airways (the lungs). When infections get into the lungs they can cause pneumonia which in some cases can progress to acute respiratory distress syndrome (ARDS) requiring intensive care. ARDS is a chief driver of C19 mortality.
In prior Weekly Briefings, I have noted that over the course of the pandemic, new variants have been progressively more transmissible but not more (and possibly less) virulent. This was most apparent with Omicron which causes extremely high case rates but comparatively low death rates wherever it strikes.
Viruses survive by spreading, making transmission a virus’ chief imperative. When a virus has spread widely throughout its host population, it comes up against impediments to transmission–chiefly, prior immunity. Eventually, if enough people have had the virus, a population can develop ‘herd immunity’ preventing the virus from being able to continue to spread.
This puts evolutionary pressure on the virus to mutate in ways that make prior immunity less effective (immune escape). As a virus evolves into new variants that can evade prior immunity, it has the ability to begin reinfecting those who were previously infected, enabling it to start spreading widely again even among a population that has wide population-level prior immunity.
As the virus shape-shifts to circumvent prior immunity, this also affects how it acts inside the body including the clinical disease it causes. Omicron, for example, mutated in ways that have enabled Scov2 to infect both vaccinated and previously infected people at a very high rate while also causing less pneumonia and less loss of smell. Omicron produces more mucous and this is likely helping it to spread not just through the air but through touch (fomite transmission).
If future variants were to continue in this line, C19 could eventually become a disease more like a cold or flu. However, as discussed in a new paper in Nature, selective pressure on viruses to evolve toward better immune evasion does not guarantee that the side effect will be lower virulence. In fact, it could go the other way–to become more deadly. And the jury is still out as to whether BA.2, BA.2.2, and BA.2.3 have higher, lower, or the same level of virulence compared to Omicron.
How does the US compare to SK and HK? Like HK, the US has a relatively low vaccination rate with only 29% of the population boosted and just 65% having received primary vaccination (2 shots).
Like in SK, BA.2 also now accounts for about 23% of cases in the US. But that number is growing rapidly and BA.2 or BA.2.2 will likely be the dominant variant in the next 2-3 weeks. That could indicate that the coming wave of BA.2/BA.2.2 in the US might cause higher case mortality rates than those seen in SK.
On the positive side, in the US, we have a high rate of vaccination among those over 70 (about 90%). Of all the factors impacting the case fatality rate, vaccination among the elderly is probably the most important. This has been born out through the Delta and Omicron waves and will likely hold true as we go through the next (hopefully smaller) wave caused by BA.2/BA.2.2.
People who have had Omicron are likely to have some degree of protection against BA.2 infections and after the recent enormous wave, that’s a bit of good news, too. However, we don’t yet know how much protection Omicron will offer against BA.2 or BA.2.2/BA.2.23 and there are already studies and case reports showing that people who got Omicron can be reinfected just a few weeks later with BA.2. In addition, neutralizing antibody titers post-vaccination are significantly lower against BA.2 than Omicron. Those who had prior variants including Alpha and Delta are not well protected against either Omicron or BA.2.
Also, despite faulty predictions from some public health experts that everyone in the US would contract C19 during the Omicron wave, the CDC recently estimated that to date, only about 43% of Americans have been infected by the Scov2 virus (all variants combined) with about one-fourth of those cases caused by Omicron. That leaves the vast majority of the US population vulnerable to BA.2/BA2.2 which might or might not be more virulent than Omicron.
Here’s my take: Across the world, we are seeing new waves of cases being caused mostly by BA.2 and BA.2.2. Throughout the pandemic, the pattern of case waves in the US has followed those seen in the UK by a few weeks. The Alpha, Delta, and Omicron waves in the US all began about 4 weeks after those in the UK.
Right now, the UK is experiencing a sharp rise in cases that looks similar to that seen in SK, HK and elsewhere.
As discussed at length in previous Weekly Briefings, public health experts in the US have decided to follow the UK, Denmark, and other countries in adopting a new pandemic strategy that prioritizes protecting hospitals and preventing deaths at the exclusion of preventing infections.
As such, like in the UK and Denmark, because Omicron has a lower propensity to attack the lungs and is, therefore, less virulent, extremely high-risk activities such as indoor restaurant dining, bars, concerts, etc., are now permitted almost everywhere in the US with no vaccination or masking requirements whatsoever. What could possibly go wrong?
In a recent Weekly Briefing, I discussed the addition of Scov2 wastewater surveillance as one of the four critical tools needed for us to emerge from the pandemic. As of the end of last week, 37% of wastewater sites monitored by the CDC have seen an increase of 100% or more in Scov2 levels in wastewater, mainly clustered around cities in the Northeast. About 30% of those sites showed an increase of 1,000% or more.
With the US vaccination rate lower than that in SK but with better vaccination coverage among the elderly compared to HK, we should prepare ourselves for a wave of cases caused by BA.2/BA.2.2 with a death rate that is higher compared to SK but lower compared to HK. The hospitals will likely hold and that, it seems, is what matters the most to the US public health authorities.
III. Studies and other announcements of note this week
1585. No surprise here: A new study from the UK shows that longer interdose intervals (12 weeks between the first and second doses) improved vaccine protectiveness in the real world against infections by producing higher antibody responses and that Pfizer performed better than AstraZeneca.
https://www.nature.com/articles/s41467-021-27410-
1586. 28% of hospitals in the State of California anticipate critical staffing shortages in the next week.
1587. New research from Hong Kong shows that Omicron can survive on stainless steel, plastic, glass and paper for up to one week–much longer than prior strains which could survive up to a couple of days. My note: This evidence adds to my sense that Omicron (and BA.2) may be spreading more quickly in part because, unlike prior variants which were spread mostly through aerosol transmission, the new variants, which produce more runny nose/mucous and can survive longer on surfaces, are also being spread widely through touch (fomite transmission). Let’s keep washing our hands!
https://www.biorxiv.org/content/10.1101/2022.03.09.483703v1.full.pdf
1588. The algorithm currently being used by the CDC to rate community level C19 risk has changed again. It includes 7-day averages for:
Cases per capita
Hospital admissions per capita
Share of inpatient beds for patients with C19
https://www.cdc.gov/coronavirus/2019-ncov/science/community-levels.html
1589. According to the new algorithm, San Diego has been instantly downgraded from a county of substantial risk to one of low risk:
https://covid19florida.mystrikingly.com/national-community-profile