COVID-19 Weekly Briefing for Monday, February 28, 2022
HCOV vaccine, antivirals, RATs, and wastewater surveillance
COVID-19 (C19) Weekly Briefing for Monday, 2/28/22, in summary:
Wastewater surveillance is the fourth column of the pandemic strategy; new CDC guidance contradicts the California Department of Public Health’s (CDPH) recent lifting of mask mandates for cities like San Diego; booster update; Omicron/BA.1 and BA.2 update; new multimorbidity patterns can predict C19 disease progression; genetic factors impact C19 severity.
1470 - 1480. Over the last year, I have dedicated several of the Weekly Briefings to discussing a possible path forward, out of the pandemic. My focus has been on three main things:
1. Pan-human beta coronavirus (HCOV) vaccines that can protect against a host of infectious viruses including the ones that cause SARS, MERS, COVID-19 (C19), and common colds. All HCOVs share conserved epitopes–areas on the viruses’ genetic skeleton that mutate little or not at all over time. Since these conserved epitopes don’t change over time, vaccines that target them could provide longer-lasting protection, variant after variant.
HCOVs enter the body mainly through the nose and mouth where they colonize mucous membranes in the airways and sometimes the intestines. Traditional vaccinations injected into a muscle in the upper arm train the internal compartment of the immune system to fight off the virus (general immunity)–but only after it has made its way past those mucous membranes into the interior where it can cause infection.
An HCOV vaccine administered orally or intranasally, rather than intramuscularly (IM), would not only be more durable, it would train the part of the immune system that defends the airways and gut. This is known as mucosal immunity.
Part of mucosal immunity involves the production of specialized antibodies called IgA. The job of IgA is to patrol the mucous membranes of the airways and intestines where HCOVs first colonize. If a virus is swallowed or inhaled and latches on to those mucous membranes, IgA can spot it and shut it down quickly, before it has a chance to penetrate into the body’s interior to cause infection. Therefore, an intransasal or oral vaccine that induces mucosal immunity should be able to provide better protection against infection than one delivered via the traditional IM route.
At least two such HCOV vaccines now exist and the results of early clinical trials are extremely exciting. One is in pill form and the other in nasal spray form. Both can induce mucosal immunity and both appear to be significantly more effective at preventing infections than even the current (amazing) mRNA vaccines which are administered IM.
2. Antiviral medicines. Aside from the various monoclonal antibody therapies which currently have the limitations of being somewhat variant-specific (most are no longer effective against the highly mutated new variants), are hard to build to scale (and so have always been in short supply), and must be infused intravenously (further limiting access to patients), there are now at least three effective antiviral agents capable of shortening the duration and severity of infections, reducing viral loads to minimize transmission, and, if administered early enough, possibly preventing long-covid (LC) and/or organ tissue damage that may result in delayed-onset illness and disability. They are: paxlovid, NONS, and molnupiravir.
a) Pfizer’s paxlovid interferes with SARS-CoV-2 (Scov2) viral replication by inhibiting a protease (an enzyme that helps break down proteins) which the virus needs to make copies of itself. It has been shown to lower the risk of hospitalization and death by about 90% and early studies show that paxlovid can be used prophylactically to prevent symptomatic infections. It is administered as pills taken twice daily for five days along with an anti-HIV medicine (ritonavir). Pfizer has announced that it is also working on a nasal spray preparation for paxlovid that would enable faster therapeutic action by applying the medicine directly to the source.
b) SaNotize Research Corp’s NONS is a nasal spray preparation containing nitric oxide. Self-administered directly into the nose (two sprays per nostril, six times a day for seven days in clinical trials), NONS reduced Scov2 viral load by more than 94% within 24 hours of treatment, and by more than 99% in 48 hours.
It is inexpensive, can be manufactured to scale quickly, has been shown to reduce the disease course of C19 in half (4 days compared to 8 for controls), and is already available for use in Israel, India, and elsewhere, including New Zealand, where it is available over the counter.
Like paxlovid, NONS can be used prophylactically to prevent colonization of the virus in the nose and throat or abortively to halt colonizations from progressing to infections.
Unlike paxlovid, NONS does not interact with other medicines. Nitric oxide (NO) is synthesized from the amino acid L-arginine in nearly every type of cell in the human body. NO is an important molecule for blood vessel health. It relaxes arterial walls to help increase blood flow and lower blood pressure. NO synthesis is suppressed in diabetics which increases their risk of hypertension. The NO molecule released from the NONS product is identical to the one delivered in gaseous form to treat persistent pulmonary hypertension and Blue Baby Syndrome in newborns. (I am currently trying to purchase NONS from Israel, where it is sold as Enovid, for the practice.)
3. Rapid antigen tests (RATs) can help us keep better surveillance and screen attendees of social and work events such as parties and meetings. Properly used, RATs can lower the risk of congregate group activities as, state-by-state, mask mandates are being (foolishly, prematurely) lifted in the context of high community transmission.
RATs are also critical to our strategy for ending isolation/quarantine which is as follows:
Isolation/quarantine for 5 days from the date of the first positive test, the onset of symptoms, or beginning the day after a known/suspected exposure, followed by daily use of RATs, beginning on day 6. RATs should be administered using the combined throat and nose swab technique in the middle of the day as described in prior Weekly Briefings. Negative RATs two days in a row = end of isolation/quarantine.
This week, I would like to discuss a fourth measure that will likely play a critical role in helping us emerge from the pandemic. Scov2, the virus that causes C19, is shed through feces and can be detected in sewage. Evaluation of wastewater for Scov2 offers the ability to both quantitatively and qualitatively surveil communities for C19–two things that are critical for ongoing response planning.
As fewer people seek C19 PCR tests because they are less available and no longer free, it is becoming increasingly difficult to rely upon the average daily case rates reported by local public health deparments to assess community prevalence and risk. Currently, based on the best epidemiological modeling, I have been multiplying the SDDPH reported average daily case rate by five to estimate the true local case rate, day by day. But it is hard to know how accurate an estimate that truly is.
Understanding community prevalance is a critical element of risk assessment. When case rates are high, so is the risk of infection associated with normal activities of daily living; when they are low, the risk goes down. Monitoring wastewater has emerged as the most sensitive and accurate method for detecting both upticks and downturns in case rates as well as for genomic surveillance.
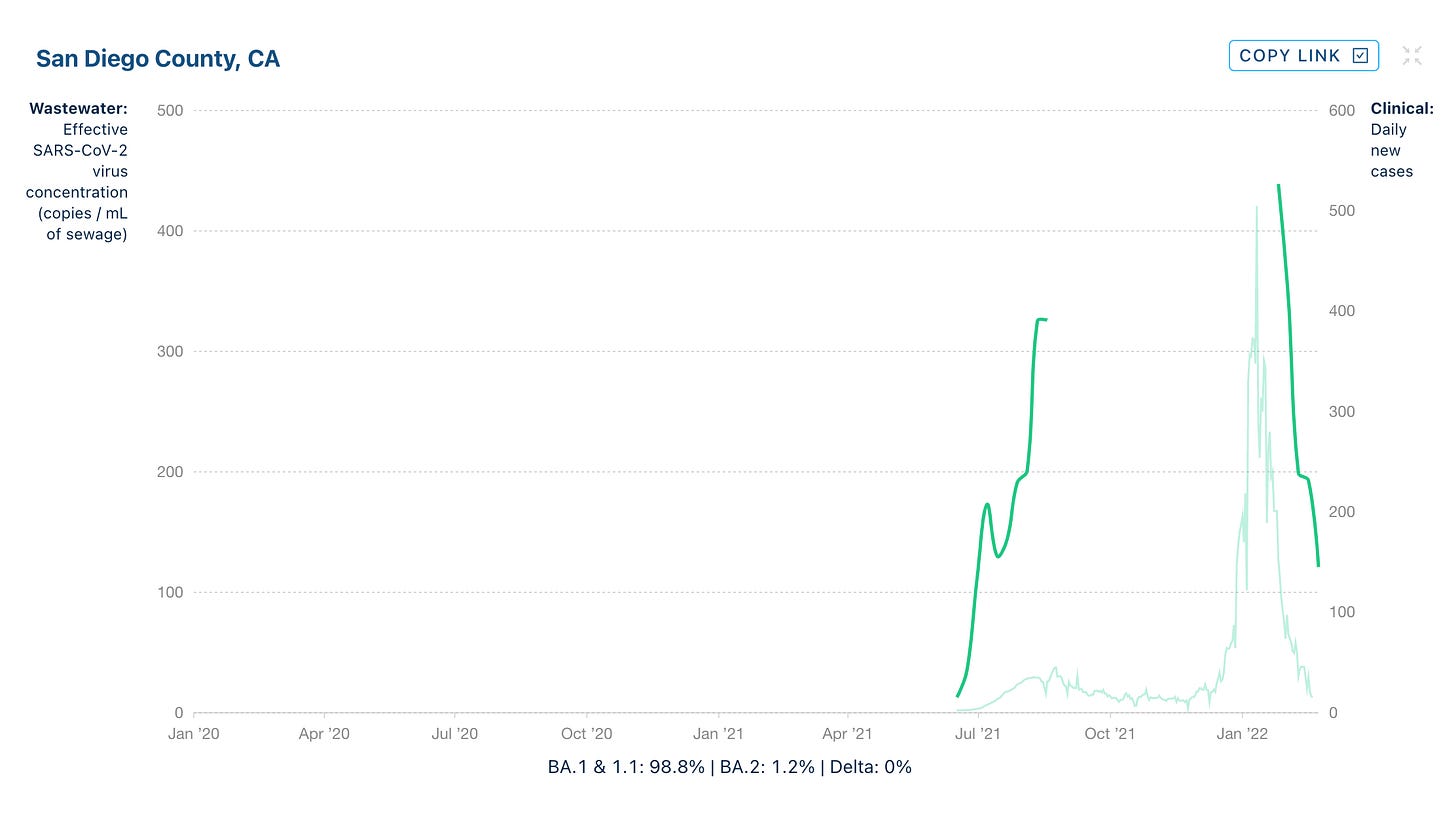
As reported in prior briefings, UCSD has been at the forefront of predicting waves of C19 disease through wastewater testing. Using an automated wastewater concentration process that employs liquid-handling robots, this method has been shown to be extremely sensitive, capable of detecting one asymptomatic individual in a building of 415 residents. Because the virus is shed in stool well before PCR testing is performed, analyzed, and reported to the CDPH, and often before (especially under-immunized) people first develop symptoms, this high-throughput method can be used to forecast C19 cases at least a week ahead of PCR testing with extreme accuracy, and three weeks ahead of time with fairly high accuracy.
For example, as previously noted in the Weekly Briefings in mid-December of last year, UCSD School of Medicine reported the steepest rise in wastewater Scov2 RNA titers since the beginning of the pandemic. Genomic investigation revealed the presence of the Omicron variant, confirming the suspicion at that time that the new VOC had made its way to San Diego.
This was valuable data that helped our office plan for what was coming by reverting to the strictest transmission mitigation protocols which we continue to employ currently. We added the use of face shields to our N95-equivalent masks, went back to opening all doors and windows (even though the weather has swung back in forth in wide arcs of relatively extreme hot and cold temperatures), discontinued the performance of on-demand PCR testing, and increased our telemedicine encounters.
On the basis of the wastewater data, UCSD was able to correctly predict that the Omicron wave would likely be the largest to date. Indeed, it dwarfed all prior waves, peaking about a month later in mid-January, with average daily case rates approaching 15K (by comparison, the Delta wave in San Diego peaked in early July with an average daily case rate of just over 2K). This is a good example of how wastewater data preceded the official recognition of the Omicron wave based on clincally reported cases confirmed by PCR testing by almost 3 weeks.
As some of you may have noticed, the CDC has finally begun including wastewater Scov2 RNA titer data being collected from various communities across the country. It’s a step in the right direction, although, as you will notice, the data are difficult to segregate in a usable way and do not include genomic surveillance/investigation. A better source (sadly) than the CDC can be found here collected by Biobot Analytics. These data can be easily segregated not just by region or state but by county.
For example, here in San Diego County, the SDDPH reported average daily case rate is a little over 1K/day. Multiplying that number by five gives me an estimated true rate of about 5K cases/day. On that basis, the number of cases is now declining sharply from the peak but is it trustworthy? How does that estimate square with wastewater testing data? Biobot resumed wastewater data collection at the end of January and we can see that Scov2 RNA titers are dropping precipitously in San Diego County, in tandem with the reported average daily case rate based on clinical (PCR) testing. This gives some assurance that the dop in reported cases is not merely an artifact of fewer tests being sought out.
The end of the pandemic will probably not come suddenly as was hoped when the awe-inspiring vaccines were first rolled out and shown to be highly protective against infections by the Alpha variant (and there was a reasonable expectation that everyone would want that protection). Rather, it will more likely come gradually as we reach a balance point between technological evolution affording better protections (see above) and Scov2 evolving to become (hopefully) less menacing.
Of course, these outcomes are not guaranteed. We are yet to see the last variant of Scov2 and it is possible that the trend toward lower virulence could reverse itself. As selective evolutionary pressure on the virus moves it toward greater degrees of escape from prior immunity, a wide range of potential outcomes presents itself.
But as new variants emerge and make their way around the world, wastewater surveillance will provide us with the data we will need to more nimbly tighten and loosen transmission mitigation protocols in response to community prevalence. We will be able to spot new variants quickly. And we will be able to use the wastewater data in paralel to the clinical (PCR) testing data to make risk calculations. This is the fourth measure in the strategy to wriggle free from grip of C19.
In the meantime…
1481 - 1482. The CDC updates its risk and masking recommendations, both of which are linked to local case rates plus the estimated strain on the healthcare system (based on the number of people hospitalized and in ICU care). This is the CDC quadrupling down on their decision to prioritize hospitalizations and deaths over infections, in flagrant disregard of both LC and the potential late-term effects of organ tissue injury experienced by a high percentage of those who experience mild or moderate acute C19 disease. They only recommend masking when generalized risk, balancing case rates with hospitalization rates, is high, not when it is medium or low.
With regard just to the risk of transmission, they offer one additional layer of stratification, breaking it down into high, substantial, moderate, and low. They define high risk as > 100 cases/100K population per week or a positive PCR test rate of at least 10%, and low as < 10 cases/100K or < 5% test positivity.
Where is San Diago currently ranked in terms of general risk? High:
So, according to the CDC, everyone should currently be wearing well-fit, high-efficiency masks indoors. I don’t know whether or not any stores, theatres, gyms, or other businesses in San Diego plan to require masking based on this new guidance. Technically, it is the CDPH that has the final word.
Boosters now!
1484. Japan delayed the rollout of third doses of vaccine. They had originally scheduled boosters for 8 months post-second shot, then shortened the wait to 6 months. In the interim, the Omicron wave swept across the country and caused the largest number of daily deaths since the pandemic began. With only about 10% of the population having received booster shots, we see that Omicron, while less virulent than prior variants, is not a cold. For patients waiting to get their third shot, this data might be a cautionary tale.
1485. Despite having led the world effort to develop and distribute C19 vaccines, we currently rank 67th in the world in terms of percent of the population having had two shots and 54th for 3 shots.
1486. And the rates of infection and deaths show it. We are faring worse than our neighbors to the north and south, worse than Europe, Japan, and the UK.
1487. Of course, our bad outcomes are not solely due to vaccine-refusal fueled by conspiracy theories and other forms of political disinformation. Some of it has to do with the overall health of Americans who lead the world in obesity and chronic illness.
A new high-powered study from Spain shows that patterns of C19 illness among those with several chronic preexisting diseases (multimorbidity) are, along with age, sex, and genetic factors (see below), a strong predictor of disease severity.
Specifically, diabetes in older women (present in 99% of those who progressed to severe disease) and obesity in older men (also present in 99% of those progressed to severe disease) were drivers of hospitalizations and deaths. In younger adults, anxiety was predictive especially when coupled with menstrual dysfunction in women or atopic dermatitis in men.
If this was not such a high-powered study (approximately 50K subjects) I might have regarded some of these findings as curiosities to be watched and not included it in the Weekly Briefing. But, as previously discussed in several of the Briefings, chronic low-grade inflammation associated with cardiometabolic diseases and obesity does not only lead to atherosclerosis and insulin resistance, it is a likely driver of immune dysregulation including the cytokine storm that can lead to acute respiratory distress syndrome (ARDS) and death.
Worth a read and worth remembering that men who are obese, women with diabetes, and anyone with anxiety (especially coupled to menstrual dysfunction and atopy) should be watched more closely.
https://pubmed.ncbi.nlm.nih.gov/35181720/
Omicron/BA.1 and BA.2 update
1488 - 1497. As reported in a prior Weekly Briefing, Omicron (a.k.a. BA.1) was outcompeted by a new variant of the same lineage, called BA.2. Yet another variant, called BA.3 has also since been identified. BA.1 differs from BA.2 by 50 amino acid mutations–about twice as many as the sum total of all the mutations on Alpha, Beta, Gamma, and Delta compared to the original wild-type (Wuhan-Hu-1) variant.
BA.2 has outcompeted BA.1 in Denmark, South Africa, India, Philippines, Sweden, and Austria, and it seems to be starting to take over in the UK, Germany, and Israel, though not yet in the US.
A recent study in a lab using an animal model suggested that BA.2 is more disease-causing and more immune-evasive than BA.1. And it (BA.2) has spread rapidly in many countries as previously noted. However, the real world data so far do not support higher levels of virulence or more escape from vaccination-induced immunity compared to BA.1.
BA.2 is not gaining on BA.1 in the U.S., but the explanation for this remains elusive.
It does appear that BA.2 can cause reinfections in those who had BA.1 but it is rare (BA.1 infection looks to provide about 95% protection against reinfection with BA.2, at least in the very short-term), mild, and mostly among unvaccinated.
Finally, sotrovimab, the only monoclonal antibody (mAB) therapy effective for treating C19 caused by Omicron/BA.1, is not effective against BA.2. However, the FDA has just granted emergency use authorization (EUA) for a new mAB, bebtelovimab, that inhibits both BA.1 and BA.2 (at least in the lab).
_____________________________________________________________
1498. In a small study, gargle and intranasal administration of iodine reduced viral loads in the noses of patients with mild C19. My note: until we have better antiviral nasal sprays widely available, it makes sense to gargle and do nasal applications or lavage in patients with known exposure or infection to potentially reduce viral load in the nose and throat. I am trying to source NONS for the office.
A brief synopsis of genetic risk factors in C19
149 - 1504. It is widely accepted that, aside from vaccination/prior immunity status, the most important risk factor in the development of severe C19 disease and death is advanced age. It also appears that men seem have a slightly higher mortality risk compared to women; obese (especially obese men) higher than non-obese; those with certain comorbidities including diabetes (especially among women) and anxiety (especially coupled with mentrual disorders in women and atopic dermatitis in men) are more likely to wind up very sick compared to those without them. And there are early signals that those with asthma may be more likely to develop long-covid (LC) (see January 31, 2022 Weekly Briefing; #1403).
It also appears that genetic factors may play a role in both susceptibility to infection and disease progression. Earely Weekly Briefings from 2020 included discussions of obervational data showing that people with blood-type O and those who are Rh-negative might be less susceptible to infection with Scov2 compared to non-O and Rh-positive people, and possibly that those with blood-type A, though more susceptible to infection, might be less susceptible to progression toward severe C19 disease. This is not yet settled science as there have been conflicting reports but a pattern has formed which is both interesting and may be potentially useful in terms of assessing individual risk.
More persuasive data show that a variation within a specific region on chromosome 3 is associated with developing severe C19 disease. This particular genetic variation appears to have been inherited from humans that lived contemporaneously alongside Homo sapiens until about 40K years ago. Specifically, the Neanderthals and Denisovans of Eurasia (who engaged in some interbreeding with Sapiens) developed genetic adaptations to infectious RNA viruses.
The particular variation on chromosome 3, inherited from Neanderthals (approximately 16% prevalence among modern Europeans and 50% among Southeast Asians), appears to put modern humans at increased risk for ICU care if they get infected with Scov2. Meanwhile, another variation, also inherited from Neanderthals, this one on chromosome 12, offers 22% protection from progression to severe C19 disease.
And now, we find out that the same genetic variation on chromasome 3 that makes modern humans more susceptible to progression toward severe C19 disease, inherited via genetic flow from Homo neanderthalensis, is approximately 27% protective against HIV infection. These regions on chomosomes 3 and 12, which encode proteins that activate enzymes important during infections with RNA viruses, including the expression of cytokine receptors, are shedding more light on the field of immunology which is expanding at unprecedented speed–part of the silver lining to the cloud that is the C19 pandemic.