The Concept of Hormesis
Finland has the highest rate of Type 1 diabetes (T1D) in the world, among children, with a prevalence of 64/100K. T1D is an autoimmune disease in which the body’s immune defenses wrongly identify insulin-making cells in the pancreas as foreign entities and attack them. But this extraordinary rate of T1D is a relatively new phenomenon in Finland where the prevalence of that disease has quadrupled since the 1950s.
In fact, over the past half-century, most countries in the industrialized world have seen stunning increases in autoimmune and allergic diseases including T1D, lupus, rheumatoid arthritis, and celiac disease, while in poorer, less developed countries, these serious health problems have remained relatively stable and rare. In Russian Karelia, for example, the rate of T1D is just one-sixth that of Finland, even though it is just 175 miles away. The people of Karelia are ethnically the same as their Finnish neighbors, so the difference between the two is not based on genetics. They share the same weather, latitude, and mostly the same diet as well. What’s different between these populations is that the residents of Karelia are comparatively poor–earning on average about 15 cents on the dollar compared to Finns. And people who live in poorer (typically more rural) areas tend to have a lot more contact with dirt.
As we learn more about human immunity, it is becoming clear that our ability to mount a robust and well-coordinated immune response to infections as adults depends substantially upon the frequency of our exposure to pathogens–especially early in life. In this sense, the immune system is like the musculoskeletal system in that the more you use it, the stronger and better coordinated it becomes. Bacteria, viruses, and parasites found in dirt are stressors that force the body to defend itself. Working out at the gym three times per week makes us gradually fitter, and routinely fighting off infections helps our immune system to grow stronger and learn how to better calibrate its defenses.
Hormesis is the concept of strengthening health through repeated exposure to things that stress our systems in a particular way. Exercise is an example of a hormetic practice. It stresses heart, lung, and muscle tissues, forcing them to grow stronger in order to meet the repeated demands of hard work. This is hormesis at work.
There are many forms of hormetic practice. Exposure to extreme cold (cryotherapy, cold plunges) or heat (sauna bathing, whirlpool), fasting, and physical work have all been shown to improve both lifespan and healthspan. In a prior Weekly Briefing, I presented research showing that people exposed chronically to low-dose radiation in the form of serial X-rays, long-distance air travel, or from living in parts of the world with higher levels of natural background radiation, actually have a lower-than-average risk of developing cancer. And there is reason to believe that regular exposure to germs helps give the immune system the workouts it needs to stay strong.
It is now understood that in the first few years of life, as with the ability to learn languages and walk on two feet, our immune systems undergo intensive self-organization as they learn how to coordinate the various cells and humors that are part of immunity. If, during that learning period, we are not exposed to germs on a regular basis, our immune system fails to grow strong and coordinate itself properly. In some cases, when there is little exposure to bugs, our young, over-eager immune systems can begin to turn their attention toward the body itself leading to autoimmune diseases such as T1D. Finnish children may, in fact, be victims of a culture that, in an effort to prevent infections, practices just a little bit too much cleanliness.
By this theory, in places where people have higher levels of exposure to dirt and therefore, to pathogenic microorganisms, especially early in life, we should, on a population level, evidence of more robust and better-coordinated immunity in the form of lower hospitalization and death rates from common infectious diseases.
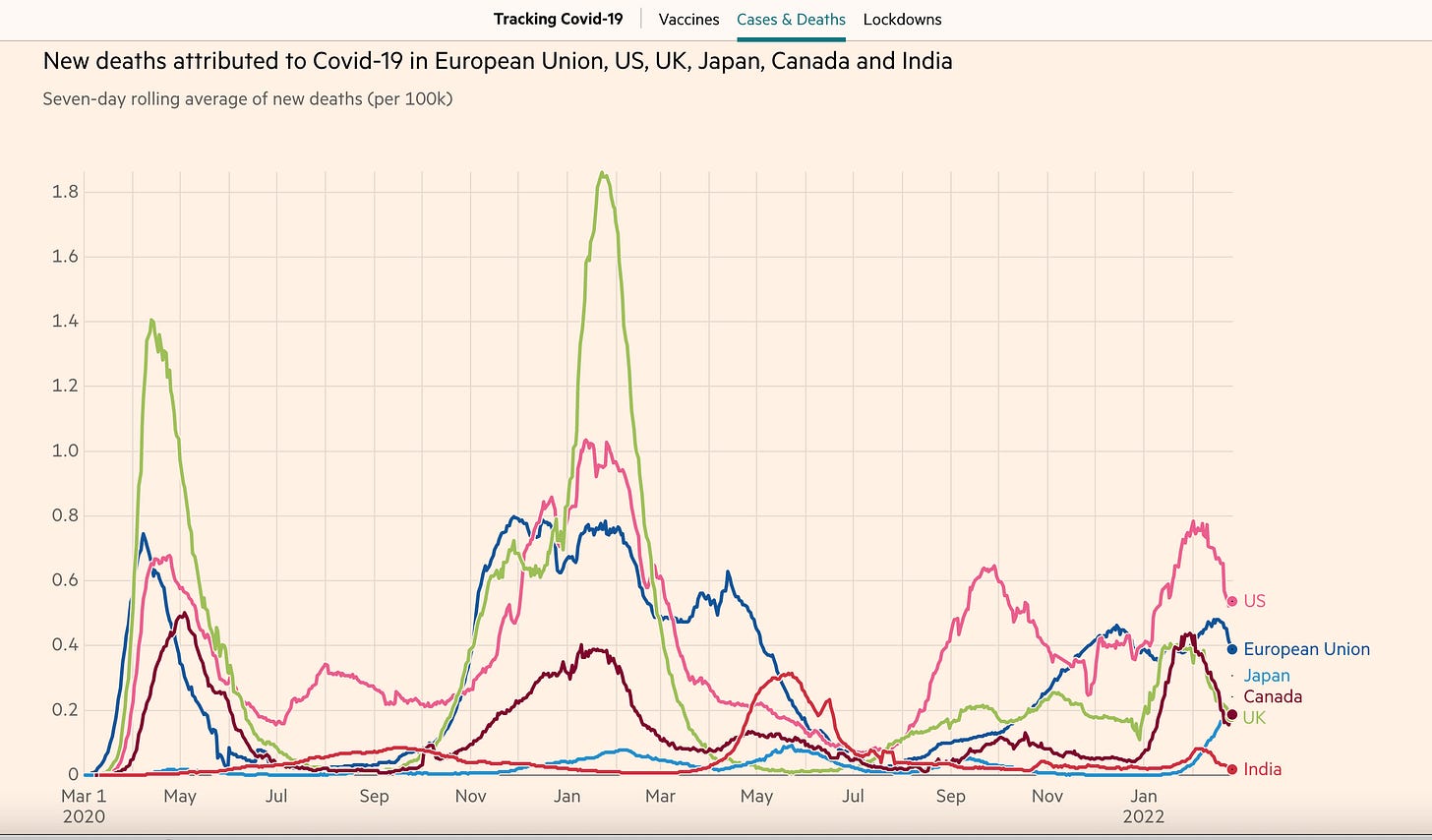
Let’s look at that using COVID-19 (Covid) as an example. India is on track to become the world’s most populous country with over 1.4B people clustered in extremely dense urban and vast rural settings. They have a sophisticated modern healthcare system that operates in their major metropolitan centers but state-of-the-art care is inaccessible to a large swath of the (especially rural) population. These things should make India highly susceptible to catastrophic loss of life in the face of an extremely contagious and deadly novel pathogen like SARS-CoV-2 (Scov2)–the virus that causes Covid. So how did India fare with regard to Covid compared to more developed countries? Better. Much better:
In fact, here is a comparison of the Covid mortality rate in the US compared to the world’s four poorest countries, Burundi, Somalia, Madagascar, and Mozambique, where public health infrastructure is minimal, vaccination rates are extremely low, and people, because of poverty, have more contact with dirt:
It is a compelling theory that exposure to dirt (especially early in life) is hormetic and that stronger population-level immunity in impoverished countries where people have had more exposure to pathogens is keeping their mortality rates low.
How should this inform us as? Here’s my take: There is a balance point for virtually all things, including health, in which ideal outcomes are favored. Exercising too much can cause injuries but not exercising enough makes our bodies weak and deconditioned. Eating too much can cause us to become overweight but insufficient nutrition can cause deficiency states that lead to disease. In a nutshell, too much stress on the system can break it but too little can leave it weak and vulnerable.
It is likely that in modern industrialized countries like the US (and Finland), efforts to create sanitary environments, including the excessive use of antimicrobial agents, have resulted in a kind of hygienic overshoot. Protecting our children (especially infants and toddlers) from any exposure to pathogens is considered good parenting practice. But it might very well be training them to become immunologically weakened and/or dysregulated adults, leaving them more vulnerable to autoimmune, allergic, and infectious diseases.
What happens when societies start choosing to ignore less deadly variants?
As discussed at some length in the 1/31/22 Weekly Briefing, Denmark lifted all public health mandates on Feb 1, 2022, despite rising case levels of Covid caused by the new variant, BA.2. Currently, in Denmark, you can test positive for Scov2 infection and still go to work unmasked, eat in restaurants, attend the theater, laugh, shout, sing, cough, sneeze, and engage in up-close conversations with friends, family, coworkers, and strangers–all at your own personal discretion.
Why would Danish public health authorities and the Danish government do such a thing? When they made this decision, the mortality rate had started to come down even as case rates were still climbing–critical data informing the now-familiar strategy of prioritizing preventing severe outcomes to the exclusion of preventing infections. With about 81% of the country ‘fully vaccinated’ (2 shots using the CDC terminology) and close to 100% of seniors boosted, they made the case that mild or moderate Covid was an acceptable risk when balanced against the economic, psychological, and emotional toll of pandemic behavioral restrictions.
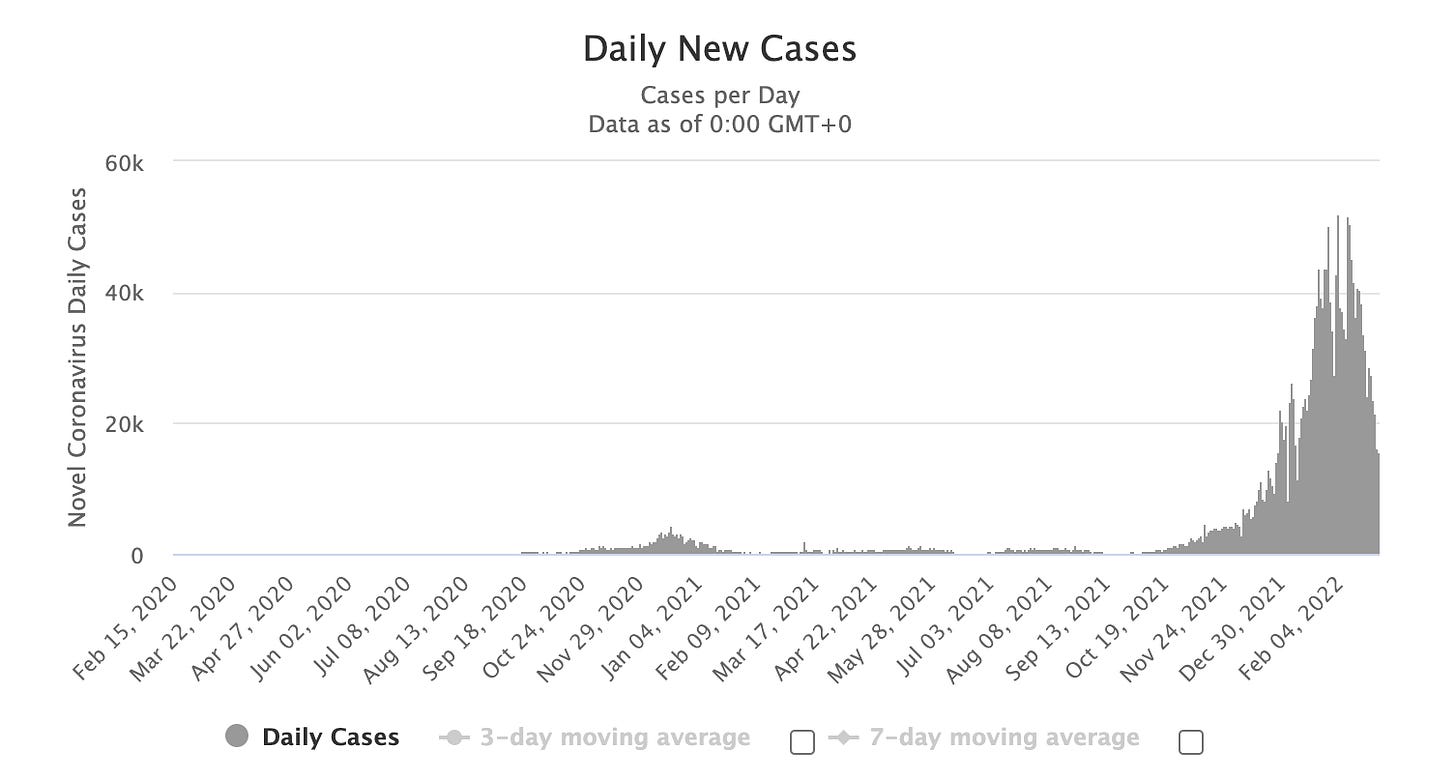
How did the mortality rate in Denmark change after removing all restrictions? Not for the better:
Allowing Covid to spread unchecked led to a ten-fold increase in mortality rates compared to any point during the last year. This, despite the now well-established lower level of virulence associated with Omicron (BA.1) and BA.2. Average daily case rates peaked at an astonishing level of > 50K (in a country with a little under 6M people).
But this may not be the whole story…
For two years now, the forces of political disinformation have been promoting the false narrative that deaths among people with Covid are not the same thing as deaths from Covid and that the officially published mortality rates from public health departments around the world are misleading–part of a conspiracy to scare people into needlessly receiving vaccinations. How do we know that this is a false narrative? By comparing the average mortality rate during the years prior to the pandemic to the mortality rate during the years of the pandemic.
When there is a higher-than-average mortality rate in a particular year, the deaths above the average are referred to as excess mortality. Over the last two years, we have seen far fewer deaths from common causes like influenza (flu) and other infectious diseases as many people have been working from home and following infectious disease risk mitigation measures such as masking and avoiding crowds. In the absence of a deadly pandemic, that should have translated into lower-than-average mortality rates. But in 2020, the first year of the pandemic, we saw the highest excess mortality rate in US history–higher even than in 1918, the year of the Spanish Flu pandemic.
And 2021 was worse still, even after the average number of excess deaths had been adjusted upward, taking into account the catastrophic 2020 data:
What’s more, the official Covid mortality rates published by public health departments worldwide do not include deaths indirectly caused by the Scov2 virus. Many sick people who stayed home rather than seeking medical attention for non-Covid illnesses because they were afraid of catching the virus at the hospital or could not access appropriate care because their local healthcare systems were overburdened, wound up dying prematurely from lack of appropriate medical attention.
In addition, only those people with PCR test-confirmed infections are included in the official Covid mortality data. People in areas where testing was limited and those who resisted getting tested for personal or political reasons were excluded from the official count. It is estimated that approximately 20% of the excess deaths in 2020 and 2021 not attributed to Covid were, in fact, caused, directly or indirectly, by the pandemic.
But it works the other way around, too. Someone with Covid might die from a car accident or flu and, using the current system of reporting whereby death within 30 days of a diagnosis of Covid is counted as death from Covid, those deaths would be falsely attributed to Scov2 infection. But, using the excess mortality data, we can see clearly that the relatively small number of false attributions of death to Covid are offset to a much greater degree by the overall lower rate of mortality from other common causes, the undercounting of cases that were never confirmed by PCR testing, and the many indirect deaths caused by the pandemic.
For example, from a statistical standpoint, influenza has more or less disappeared over the last year and a half.
Over the past two years, excess mortality data have validated the published Covid mortality data. Now, however, for the first time, we may be beginning to see less agreement between these two data sets.
As societies like Denmark lift all infectious disease mitigation measures, more people are returning to working outside the home, and congregate activities like concerts, restaurant dining, and sporting events are back in full swing, we should expect a resurgence of other common infectious diseases and, along with that, a larger share of the mortality rate–including potentially the excess mortality rate–to be attributed to non-Covid causes.
This is the case being made by the Danish government, where Omicron (BA.1) has officially been outcompeted by the even more transmissible but not more virulent subvariant, BA.2, and the hospitalization and deaths rates, while high, are being far outpaced by the rate of infections.
Rather than using the daily surveillance figures for Covid fatalities which are linked to deaths occurring within 30 days of a PCR-confirmed Covid diagnosis, the SSI (the Danish version of CDC) is now using actual death certificates which represent the clinical judgment of coroners to tease out which deaths are occurring with Covid and which are from Covid, and we are, in fact, now seeing what appears to be a growing share of deaths among those with Covid and a diminishing share of deaths from Covid.
How should we make sense of this new data? Here’s my take: Calculating what level of preventable mortality is acceptable is a complex business and a direct reflection of a society’s values. Denmark is not a country known for mistreating its citizens. It is one of the wealthiest countries in the world with gleaming infrastructure and a robust social safety net. Danes enjoy some of the best healthcare in the world. Corruption is low and the standard of living is high. It ranks high among the happiest countries in the world (second only to Finland).
The calculation they are making may or may not prove to be technically correct (let’s see where the hospitalization and mortality rates go over the next few weeks). But it is based on a strategy which, like the one we are currently employing throughout most of the US, including here in California, prioritizes preventing severe illness (overburdening the healthcare system) and death over avoiding infections.
As I have written about extensively in the Weekly Briefings, there are as yet no reliable indicators of how many people who were infected but not hospitalized or killed by Scov2 will end up paying a steep price in terms of their future health, longevity, and productivity. Post-acute sequelae of Covid (PASC), also known as long-covid (LC) or post-covid conditions, are well documented and of serious concern to the CDC (although you wouldn’t know it if you haven’t spent significant time scouring their website). And, in addition to chronic illness arising directly from acute Covid infections, there is now a veritable mountain of data from all over the world documenting multi-organ tissue injury among those who experience even mild Covid.
In previous briefings, I have presented some of that data showing significant loss of gray matter in the area of the brain that deals with memory; significant drops in sperm count; significant loss of kidney and pancreatic function; significant increases in heart disease, blood clots, scarring in the lungs, and other disturbing findings after even mild infections.
Given that the current variants are less likely to cause severe acute illness and death, Denmark’s calculation could support their decision to lift all restrictions during a period of high case rates–but only if we accept the premise that keeping the hospitalization and mortality rates low is mainly or exclusively what matters. In my mind, in light of the data on LC and multi-organ tissue injury among those with mild or moderate infections, this is willful ignorance. When I try to imagine what it will mean to have a workforce plagued by chronic fatigue, brain fog, chest pain, widespread body aches, asthma, autoimmune diseases, heart disease, and a host of other conditions that are likely to arise out of long-covid, organ tissue injury, immune dysregulation, and possibly even chronic infection with the Scov2 virus, it doesn’t seem like good public health policy to let the virus rip just because a lower share of those infected are now dying acutely.
The Omicron wave is receding; where are we now?
In a recent Weekly Briefing (2/7/22), I discussed the dangers of loose talk in the Covid space. Included among the points discussed was the pernicious effect of some prominent public health experts promoting a narrative that Omicron, because it was so transmissible, would wind up infecting everyone. Predicting catastrophe without conclusive (or even highly persuasive) data is not in keeping with good scientific practice among public health experts. Of course, the prediction that everyone would catch Omicron was not meant to infer catastrophe. It was meant instead to set the stage for a shift in strategy–from one in which mitigating infections, though not the main objective, is still worthwhile to struggle for, to one in which all that really matters is preventing deaths and protecting the healthcare system from becoming overwhelmed.
In that Weekly Briefing, I argued that keeping to basic transmission-mitigation protocols like masking could prevent that from happening, citing Trevor Bedford’s estimate that 36% - 46% of Americans would likely be infected by the end of the Omicron wave. As we are now approaching the end of that wave in most parts of the country, the CDC has released an estimate, based on a nationwide seroprevalence study in which antibodies to the nucleocapsid protein were assayed, that about 140M Americans (about 43% of the population) have been infected by Scov2.
Vaccination produces antibodies to the virus’ spike protein, not to the nucleocapsid protein, while infections produce antibodies to both. By assaying for just the nucleocapsid protein, researchers were able to separate vaccinated people from those who have experienced infections.
My take: We didn’t all get Omicron and using false narratives to support preferred public health policy, even if effective to a degree, undermines confidence in public health experts and that may be the most important issue of all. This is likely not the last epidemic or pandemic we will face in our lifetimes.
https://covid.cdc.gov/covid-data-tracker/#national-lab
Vaccines/vaccinations update
Among unvaccinated Covid patients, the mortality predictors were:
Over 60
The presence of cardiopathy, liver disease, diabetes, neurological disorders, immunocompromised status, pulmonary disease, and kidney disease.
Among vaccinated patients with Covid, only 60+ and preexisting kidney disorders predicted death. “This is clear evidence that vaccination is effective as protection and saves lives,” said Maurício Lacerda Nogueira, a professor at São José do Rio Preto Medical School and a corresponding author of the paper.
https://www.journalofinfection.com/article/S0163-4453(22)00059-7/fulltext
Test-to-treat
In his State of the Union Address, President Biden announced the latest in a series of steps to help mitigate the pandemic, the ‘test-to-treat’ program. CVS, Walgreens, and Kroger will participate in the program which would allow patients suspected of having Scov2 infections to be tested and, if positive, prescribed Paxlovid on the spot. I called several CVS locations but no one knew about it. I was finally given the email address of the district manager and sent a message to her, requesting to know when they would begin enacting the program and which locations would be participating. Stay tuned…
My take: Test-to-treat is a great idea. In fact, it’s a model that should be considered not just for Covid, but for patients suspected of being infected with influenza (they could be prescribed Tamiflu on the spot too). Strep and certain curable STIs might also be considered for this streamlined process that could potentially streamline access to care and reduce the community transmission of common infections.
Viral transmission and new data on masks
In a study using a bioaerosol sampler, viral RNA was detected in cough aerosols in > 80% of 47 patients with influenza A and B. 35% of the viral RNA was in particles larger than 4 microns in diameter, and 65% was found in particles 4 microns or smaller.
As discussed at length in previous Weekly Briefings, we also know that a small percentage of people produce aerosols at levels orders of magnitude higher than average when they breathe or speak. These so-called ‘super-emitters’ are likely the people responsible for most of the spread of Covid. In fact, as has been discussed in previous Weekly Briefings, it is estimated that between 80% - 90% of all Covid transmission is being caused by approximately 10% of people: so-called ‘super-spreaders,’ while around two-thirds of people who get infected do not transmit the virus to anyone else.
These data support the well-documented stochastic (inconsistent) spread of Covid, including the fact that, even with Omicron, the risk of Covid transmission within households is only around 30%, with most households reporting one or no secondary infections and a small number showing everyone in the house catching it.
Here, we see how, among 38 subjects with influenza A or B, most generate tiny virus-containing aerosols (less than 5 microns in diameter), but one person, in particular, seems to be generating almost exclusively extremely tiny aerosols (less than 1 micron in diameter). These tiny particles are capable of traveling great distances and, when inhaled, can go deep into the respiratory tract to seed infection. Such a person is likely a super-emitter and therefore if infected, a superspreader
In fact, it has been estimated that the median size of exhaled aerosols during normal breathing is around 1.6 microns in diameter. However, when our breath mixes with room air, evaporation of water from these tiny droplets occurs quickly, narrowing the diameter of a typical aerosol from around 1.6 microns as we breathe them out to around 0.5–0.8 microns when we breathe them in. It has been established that Scov2 RNA is recoverable in aerosols and that most of the Scov2 RNA emitted by infected persons can be found in these very tiny aerosol particles.
Now, in a new study, we see that the filtration efficiency for smaller aerosols using woven cloth masks is extremely low (in the range 2.5%–10%) due to most of the airflow being channeled through relatively large (tens of microns in diameter) inter-yarn pores.
Surgical masks have been shown to work better than cloth masks and have previously been estimated to offer an approximately 56% reduction in transmission of tuberculosis when used as source control. And similar findings were reported with Scov2 transmission in an animal study using a surgical mask partition.
None of these studies took into consideration mask fit which, along with fabric filtration efficiency, is the other key component of protection against disease transmission. Surgical masks tend to fit loosely on the face with gaps between the mask and skin, especially around the bridge of the nose and under the chin. Persons wearing surgical masks are generally breathing in a mix of filtered and ambient air which reduces the real-world protectiveness of most surgical masks.
From the earliest days of the pandemic, with studies from China deconstructing superspreader events in congregate environments such as restaurants, Covid has looked suspiciously like an airborne infectious disease. It was on that basis that we decided to source, stock, and supply our team and all of our patients with N-95 equivalent masks, rated to reduce the risk of infection by > 95%. To date, none of our team members have contracted nor spread Covid to anyone at our office.
Covid adjacent
A modeling study shows that pre-exposure prophylaxis (PrEP) reduced the incidence of HIV infections by 53% and that early diagnosis and early use of antiretroviral therapies reduced it by 22%. The UK is now on track to eliminate HIV disease in the next 2-3 decades. Will HCOV vaccines and antivirals do the same for Covid?
In China, various wildlife species are sold as food and for purported medicinal value. Several, such as bats, camels, and pangolins, have been established as potential reservoirs for viruses that can infect humans. In previous Weekly Briefings, I presented evidence that cats, dogs, and minks can harbor Scov2. Analysis of nearly 2K game animals from 18 species, including five mammals, from across China revealed more than 100 mammalian-infecting viruses, including 65 described for the first time in this paper. 21 were considered as potentially high risk to humans and domestic animals. Here are some key points:
Civets carried the most potentially high-risk viruses.
Bat coronavirus HKU8 can be passed from bats to civets.
Other coronaviruses can jump from bats to hedgehogs, from birds to porcupines, and from dogs to raccoon dogs.
Avian flu virus (H9N2) was found in civets and Asian badgers.
There is likely human-to-wildlife virus transmission as well.
The confluence of a high number of viruses in wildlife with the potential to jump to humans and a culture that supports the trapping, selling, trading, and use of such animals for food and medicinal purposes, makes China particularly worrisome from the standpoint of the potential emergence of novel pathogens that can cause deadly pandemics. With 21 viruses identified by this group having a high-risk potential to infect humans, we should be making public health strategy now for future pandemics, including pressuring the Chinese government, which has no hesitation to crack down on its people, to disallow the practice of trapping, trading, and selling wildlife, including at so-called ‘wet markets.’ If we don’t, we’ll likely be caught on our heels again, maybe soon.